Hospice Ethiopia were honoured to have hosted an ‘Experience Sharing Meeting’ for Addis Ababa Health Bureau. A dynamic team of 20 healthcare professionals representing different sub-cities attended the meeting. Ephrem provided an overview of Hospice Ethiopia, shedding light on their main programs and the services they offer. The palliative care nurses, Kalkidan and Filagot, then shared their invaluable experiences regarding service provision, the care model, and also the challenges they face in their work.
The Q&A session was lively, where different ideas were raised, fruitful discussions occurred, and experiences were shared.
Haiminot’s story
Haiminot is a 36 year old lady with HIV diagnosed 15 years ago, and cervical cancer diagnosed 8 months ago at the Tikur Anbessa Hospital. She has been on the waiting list for radiotherapy since diagnosis, but has not had any cancer treatment to date. A single parent, her 15 year old son is in the care of her sister, who is also of very limited financial means. Her son visits about once a month. She is renting a single room (about 3m X 3m) for ETB 1,800 per month (about £28). Apart from the monthly grant from Hospice Ethiopia of ETB 1,000 she appears to have no other source of income. She had previously spent 2 months living in a church near Dessie (400 km north of Addis Ababa) hoping for a cure as someone had told her the Holy water there was good for cancer sufferers. She was referred to Hospice Ethiopia by the Tikur Anbessa Hospital.
The Hospice Ethiopia team had previously successfully treated her odorous vaginal discharge with metronidazole douches, along with tramadol for pain and bisacodyl for constipation. However, she then stopped taking all her medicines apart from her antiretroviral medication, believing that her religious faith would bring about a cure; her odorous vaginal discharge then recurred. She is now house bound with very limited mobility as she likely has nerve damage affecting her leg muscles, probably caused by the tumour. Other medical problems include anaemia for which she had previously been prescribed an iron supplement syrup which she had stopped taking and she had declined a blood transfusion on religious grounds.
Nurse Filigot spent much time listening to this lady exploring her health beliefs and emotions. She looked low in mood. Filigot negotiated for her to resume the vaginal douching with metronidazole for the odorous discharge but otherwise she continued to decline further treatment aside from her antiretrovirals. She remains on the Tewolde Medhane fund (monthly grant). She will be reviewed in a month unless she returns to the church at Dessie, and has Filagot’s phone number should she need to be seen sooner.
Hospice Ethiopia in the media!
We’re very excited to see the publication of an article written by one of our contacts in Ethiopia, Fred Harter, which describes the current state of palliative care in the country and the critical work carried out by Hospice Ethiopia. Please read the full article here. Following this Ephrem, the director of Hospice Ethiopia in Addis Ababa was interviewed by the BBC in August, for their Newsday radio program.
July fundraising
Thank you to everyone who has volunteered and supported our recent fundraising events which have raised a total of £782.50. These included a Tombola at Aldborough Fayre (£227.50), the Morgan’s tennis party (£305) (see photo), and a presentation to Reepham Rotary club (£250). This brings the total raised through events this year to a fantastic £6250 – thank you so much to all of our volunteers and supporters for raising these funds to support the vital work of Hospice Ethiopia.
July news from Ethiopia
Report from Wengi Yared, Project Co-ordinator, Hospice Ethiopia:
“I am thrilled to have successfully completed the Young African Leaders Initiative Regional Leadership Center East Africa (YALIRLCEA) Residential Programme. It was a privilege to have joined the very competitive programme as one of 3 Ethiopians in Cohort49. It has been an incredible journey, filled with transformative experiences and invaluable learning opportunities. Throughout the four-week programme, I had the privilege of engaging in experiential learning which equipped me with the necessary tools and knowledge to drive meaningful impact. Collaborating with a diverse group of talented peers further enriched experience. I look forward to applying my skills and knowledge gained during my training to drive positive change in my community and beyond.”
Links with the Pink House:
Sue and Jamie were invited to visit The Pink House in Addis Ababa during their visit to Ethiopia last February. It was set up 5 years ago as a non-governmental organisation (NGO) which provides accommodation for female patients coming to the capital for oncological treatment (mostly breast cancer and cervical cancer) who would otherwise have nowhere to stay. The patients often have advanced disease and experience highly unpleasant symptoms. We were delighted to hear that a Memorandum of Understanding has now been established between the Pink House and Hospice Ethiopia agreeing that Hospice Ethiopia will hold a weekly clinic at the Pink House to enable their patients to receive specialist symptom management.
Training for nurses working for the Addis Adaba Health Bureau:
The Addis Ababa Health Bureau have recently organised and funded palliative care training for 120 of their staff: doctors, nurses and pharmacists, with a vision to establish the provision of palliative care at health centres in the capital. The training is being provided by Ephrem Abathun from Hospice Ethiopia, Dr Henok, Dr Habtamu and one of their own staff who received training last year from Hospice Ethiopia. It is both exciting and challenging for Hospice Ethiopia to receive increasing numbers of requests from different health organisations for palliative care training. Health care professionals are increasingly realising how their patients will benefit from this type of care and we look forward to more people receiving focused symptom management in their terminal illnesses.
Training at Dessie:
Hospice Ethiopia UK has recently helped to fund training in a new oncology department at the hospital in Dessie, in north-central Ethiopia, which ran from 17th-21st July. Overall £6000 was donated – £500 from the Paradigm Norton Trust, £500 from Aylsham Rotary, and £5,000 from the Forrester Family trust. Dr Haimanot, Executive Director of Dessie Hospital, expressed her thanks for the training that will enable her staff to improve care for their patients. A total of 29 members of staff, including doctors, nurses, and hospital management, received the training. There will be follow-up and mentoring from the Hospice Ethiopia staff.
Meeting with the Ethiopian Minister for Health
The team at Hospice Ethiopia in Addis Ababa had a very productive meeting with the Ethiopian Minister for Health, Her Excellency Dr Lia Tadesse, along with other representatives from the Ministry of Health (MOH) and staff from Hospice Africa Uganda. Palliative care and opioid use for pain relief were discussed, and representatives from the Ministry of Health committed to support the re-initiation of local Morphine production. This is a crucial step as Morphine is a very effective pain-relieving drug in palliative patients and is currently unavailable in Ethiopia. The palliative care representatives at the MOH will be working with the technical advisory team, the pharmacy department at Addis Ababa University, and other pharmaceuticals in the country to assess the resource requirements and mobilization for the local production of morphine.
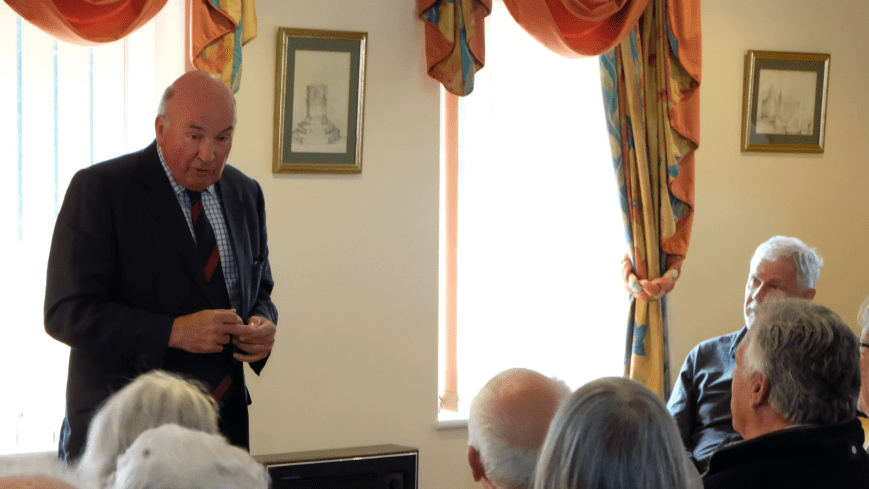
Successful talk by Lord Dannatt
Huge thanks to everyone who came to hear Lord Dannatt’s talk in June (see above photo). His talk was fascinating from responding to questions about 19th century warfare right up to analysis of the conflict in Ukraine. His insights into Putin’s Special Military Exercise were particularly thought provoking. With a packed audience an amazing £1083 was raised to support the work of Hospice Ethiopia.
Patient Story: Omari
Omari is a 40 year old male with HIV and diabetes. He was diagnosed with an abdominal tumour 10 years ago and underwent surgery. After the surgery he became partially paralysed; the exact cause of this is unknown but may be due to spinal cord compression from spinal metastases (secondary cancer). The Hospice Ethiopia team became involved in his care a year ago to control his pain and help him with his psychosocial issues. A few months ago he had a fall and since that time he has been unable to walk and so is bedbound and incontinent. He complained of pain in his legs and was prescribed a number of medications to try to control the pain; although none have been very effective.
Omari is now unable to straighten his legs and finds moving his legs exacerbates the pain; in addition he has suffered from bedsores for several months. Recently he has developed 2 new sores on his lower back which were caused by a hot water bottle as he has numbness in that area so did not realise how hot the bottle was.
He lives in a small Kebele house (social housing) with his wife and their 2 children, aged 3 and 7. His family have employed a maid to care for him. He has a strong Christian Orthodox faith and as he can no longer get to church the priest visits him at home and prays with him.
Plan: He agreed to restart tramadol for the pain in his legs. Nurse Filagot will provide a sheath (donated by Hospice Ethiopia UK) to ease the problem of incontinence. The family are currently buying pads which are expensive ETB 2,000 (£33 approximately) per pack of 24. The nurses from Hospice Ethiopia will continue to visit him regularly. Filagot had a good rapport with Yonas, listening to him attentively and quietly talking with him.
Maintaining relationships with long term supporters
Sue and Jamie have recently been meeting in the UK with some interesting contacts.
First, Dr Nuhamin Tekle, who has worked closely with Hospice Ethiopia in Addis Ababa, has been back in London continuing her studies at King’s College. This is for her doctorate researching different models for providing community palliative care in resource-poor settings. Sue and Jamie enjoyed a delicious meal with her at the Beza Restaurant in London.
Second, Sue and Jamie were delighted to host Dr Marc Clark, a Canadian palliative care doctor visiting the UK. Marc has close links with the Ayder Hospital in Mekelle in Tigray, Northern Ethiopia where there is an enthusiastic team of health care professionals wanting to develop palliative care services. This was a great opportunity to discuss how collaborative work will help improve access to palliative care across Ethiopia and show Marc some of sunny Norfolk and enjoy a game of croquet!
Ayana’s Story
Ayana (not her real name) is a 38 year old Christian Orthodox woman, who was diagnosed with HIV 9 years ago. She has been prescribed Highly Active Antiretroviral Therapy (HAART) for her HIV disease which she gets free from the local health centre. Three years ago she was diagnosed with vulval cancer and subsequently received 11 cycles of chemotherapy (after having first tried Holy water). She is now waiting for radiotherapy to control her pain, vulval swelling, bleeding and discharge. She is unable to sit comfortably despite taking tramadol 50mg twice daily for pain. Nurse Filagot talked with her about increasing the tramadol but as the ceiling dose is 50mg 4 times daily (QDS) Nurse Filagot was worried about what she will be able to prescribe when the pain gets worse (as oral Morphine is unavailable). Ayana also complained of neuropathic pain down her right leg, so Filagot decided to arrange for amitriptyline 12.5mg at night to be prescribed. Amitriptyline will hopefully help with her sleep too.
Ayana’s mobility is much reduced due to the vulval swelling and pain rendering her housebound and dependent on her family. In addition, she has a poor appetite and local skin irritation when passing urine. She lives with her parents and does not have any children. She receives food support from Hospice Ethiopia as she had stopped working as a cleaner due to the progression of the disease.